Do you ever get really bad headaches? Stomach aches? How about being the “first to get sick” every time there’s a new virus on the block? Are you quick to get emotional swings? Or, do others tell you you’re “unemotional”? Are you finding yourself overeating, using alcohol or drugs more than usual? Do you feel anxious often? How about feeling distant from your body? Ever find yourself excessively day-dreaming? Do you suffer from chronic fatigue or chronic pain? Do you experience constant or frequent physical pain no matter how many physiotherapy, massage, or acupuncture sessions you attend?
If you answered “yes” to any of the above, it could be that your body is trying to tell you about the presence of traumatic material, and you’re simply not speaking the same language. It wouldn’t be unlikely that you’ve experienced a trauma, as 70% of Americans and 76% of Canadians will have experienced a traumatic event in their lifetime; and of that population, 20% will develop Posttraumatic Stress Disorder (PTSD) (van der Kolk, 2000). If there is trauma that your body is carrying, it means you definitely need to see a trauma therapist to help you translate what your body is trying to get you to look at. If you don’t, the cost is well…a hefty one: you’re bound to spend a lot of money over time (with little to no resolution), or not be able to work and as a consequence, lose potential income; you could be missing out on having a rich emotional palate and be able to fully express yourself; and your relationships are bound to continue to suffer.
Ok, so far I’m the bearer of bad news right? Well, I know, someone has to break it to you. As a trauma therapist, people are often shocked when I tell them that part of the trauma healing process includes the resolution of physical ailments along with psychological and emotional processing—it’s all part of the same system. I discovered this phenomenon early in my adult life as I trained to become a massage practitioner. I used a deep tissue, acupressure massage technique (called Brandon Raynor Massage), and would routinely notice that my clients would access forgotten or repressed emotional content as I would stimulate the corresponding meridian line. At first, I was completely shocked and unprepared for trauma memories that would surface through the massage, and I wondered what was going on with my clients. Fast-forward a decade later, and now the correlation is clear to me.
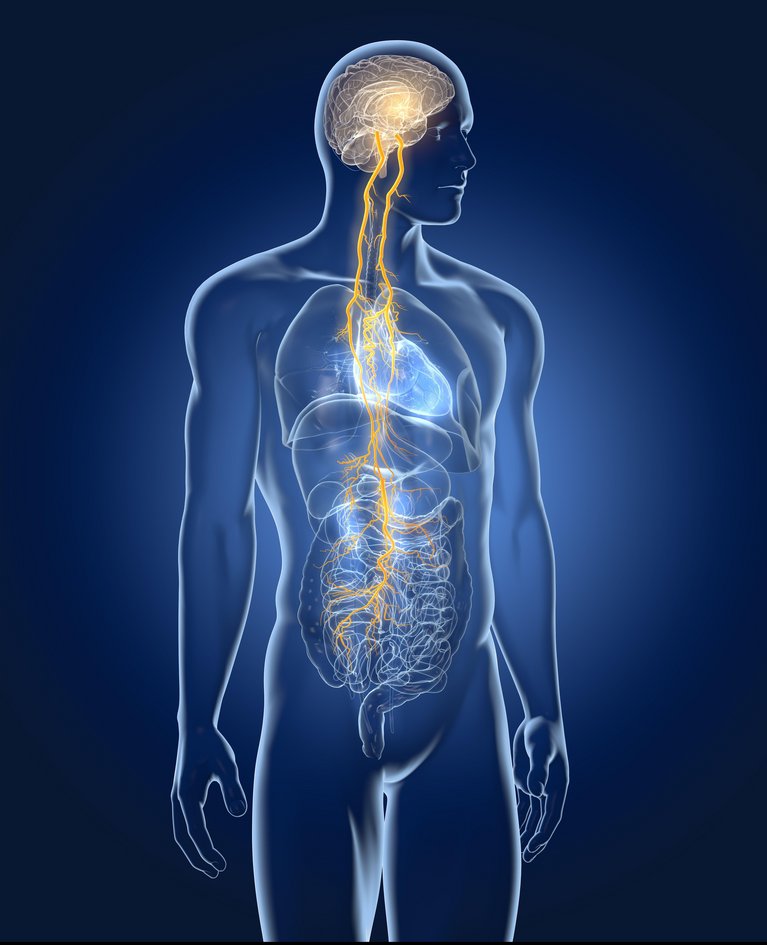
Essentially, when one experiences a trauma, aspects of the stimuli (i.e. thoughts and beliefs about oneself and the world, the five senses, and the experience of and in the body) become locked inside the nervous system and do not become processed like normal stimuli (like what you had for dinner last night, for example). Over time, new stimuli which bears a resemblance to the traumatic material, becomes linked, and begins to form a sort of “lens” that the individual sees the world through. It’s really important to stress that one can become traumatized by much more than the “obviously traumatic” events like: war, assault, sexual abuse, mugging, or terrorist attacks (for example). One can be traumatized by emotional and/or psychological distress or neglect, such as: repeated instances of shouting, neglect in childhood, having to tend to an adult’s psychological needs as a child, and many, many more. For more information on this process, check out this other article I wrote: WTF is EMDR?
If you’re reading this now, I’m betting that you’re pretty tired of any of the above symptoms that keep you from fully realizing your full, healthy potential. Or, maybe your physiotherapist or family doctor is asking that you start paying rent. Ok, maybe it’s not that bad…or maybe it is; regardless, how do you know whether your physical ailment(s) are more than just “physical?”
Here are 10 signs that your pain might actually be trauma-based:
Physiological Arousal

Trauma is a physical experience first, in that the response occurs in the body. Sometimes traumatic material can be buried so deep below the surface, that individuals that are not aware of the trauma(s), but might still be experiencing the bodily symptoms. If you experience the following physical symptoms on a pretty regular basis, there may be an underlying presence of traumatic material (Grant, 2015) (van der Kolk, 2000):
- Restlessness
- Excessive sweating
- Being easily startled by touch or noises
- Hot and cold flushes
- Nausea
- Abdominal cramps
- Aching
- Heart palpitations (fluttering)
- Dizziness and trembling
- Sleep problems including: increased night-waking, reduced sleep-time and disturbed REM sleep (fatigue increases vulnerability to pain through reduced stamina, increased sensitivity and reduced immune functioning)
- Being more prone to getting colds and illnesses
- Increased use of alcohol, drugs, and/or overeating
If you are constantly suffering from the above symptoms and you do not receive relief from traditional healthcare approaches, it might be time you contact a trauma therapist.
2. Biochemical Imbalances

Some people can develop different relationships to pain, based upon how their brain produces its biochemical interactions with other parts of the autonomic nervous system. (Grant, 2015).
When stressed, the human body produces cortisol (mostly through the adrenal glands) which provides information to the brain as to whether or not the body should “fight or flee” a potential threat to its survival. During the stress response, individuals have a higher degree of tolerance for pain (endorphins are firing, adrenaline is pumping, etc.) because it might be time to either engage in combat, or run from a saber-toothed tiger (don’t worry, I’m pretty sure they’re extinct).
Now, when the opposite affect occurs, such as in the stress system (less cortisol), the result is depression, decreased energy, and less resistance to pain (Grant, 2015). Chronic Pain sufferers have been shown to have lower levels of cortisol and substance P (neurotransmitter responsible for increasing sensitivity to pain) (Grant, 2015). The net effect is a lowered ability to resist pain, and the increased reactivity to pain (i.e. you’re always in pain, and you might as well start living at your healthcare clinic).
If you are in pain quite often (or considered to have a “chronic pain” condition), it could be that you are suffering from underlying trauma symptoms.
3. Depression and Anxiety

What if you experience pain but no doctor, physiotherapist, massage practitioner, acupuncturist, or specialist can give you a “proper diagnosis?” Did you know that ? (Grant, 2015) And did you know that almost mental health diagnoses contain a physical component to them? As many as 50% of depressed people (particularly veterans and accident victims) also are diagnosed with PTSD (Grant, 2015). Depression also tends to reinforce feelings of vulnerability and helplessness which are hallmark symptoms associated with PTSD (Grant, 2015).
Anxiety can also influence your perceptibility to increased pain. This generally happens if you’re anxious about pain. Anxiety and worry is often a concern about danger in some manifestation. Anxiety is a tool that our system uses to prepare itself for danger or the threat of danger. However, if you’re extra worried about pain, this tends to magnify the perception of danger, and leads to a higher pain perception (especially so when anxiety triggers past traumatic events) (Grant, 2015).
If you experience depression PTSD symptoms, your physical ailments may have no “medical explanations” (Grant, 2015). If you experience high levels of anxiety, you may be at an increased risk for experiencing pain.
4. Avoidance

During a trauma, our brain tries its best to protect us—many survivors of trauma report experiencing a phenomenon called “dissociation” (more on that later). After the traumatic incident, our brain still tries to protect us from the traumatic residue. It seems that because we experienced something so overwhelmingly terrible, painful, scary, and/or unavoidable (physical, emotional, or psychological trauma), our nervous system still tries to protect us from that trauma (Grant, 2015).
Trauma expert Peter Levine, states that animals in the wild shake their bodies after a trauma to discharge the negative energy. (Levine, 1997). We as humans are not usually as lucky to be able to discharge that energy after a traumatic event. We generally tend to try and “appear strong,” and “get back to normal.” In an effort to “get back to normal,” our minds figure out a way do so, dealing with the trauma. This is often through , something that anxiety promotes. While avoidance is a great coping strategy, it becomes ineffective over the long-term. (Grant, 2015).
If you ever find yourself avoiding anything like: certain topics, places, people, feelings, etc., it could mean that your brain is trying to protect you from dealing with traumatic material.
5. Dissociation

Dissociation is a natural survival response that kicks in when responding to a threat. During times of extreme stress, the brain focuses only upon survival and enters the “fight/flight” response. When the stress is outside one’s natural “window of affect tolerance,” the individual will experience “dissociation.”
Survivors of physical and/or sexual abuse are more likely to develop dissociative coping strategies to handle traumatic or painful experiences. Dissociation can also occur from emotional abuse, which can be anything from shouting, severe criticism, insulting remarks, being ignored by one’s parents, caregivers, spouse, or close attachment figure(s) for a significant period of time. People who are depressed or alexithymic (showing no emotion) are more likely to engage in dissociation as a coping mechanism (Grant, 2015).
Dissociation can be displayed by physical symptoms such as: tremors, tics, intrusions, fixed ideas, hyper-arousal, and complete re-experiences (these are termed “physical symptoms” because they are “obviously observable”) (Grant, 2015). Individuals can also experience functional losses such as paralysis, and loss of motor control (these are considered “negative symptoms” because they are often more discrete and involve “losses”) (Grant, 2015).
Depending on how severe the original trauma(s) was/is (i.e. complex trauma), the dissociative tendencies in the mind may also develop multiple layers of the personality. This means that the “everyday part” (or the “Apparently Normal Part”) of the mind that is concerned with day-to-day living is often unaware of the trauma, and exists apart from the “emotional part” of the mind (which holds the traumatic memory) (Grant, 2015). This happens so that the individual can accomplish and live a relatively “normal” life, at the cost of the individual being greatly affected by underlying trauma, and being dissociated from their emotional reality.
Trauma is almost always first experienced and expressed through the body (sensorimotor experiences). When the traumatic incident(s) occurred, often the ANP is concerned with “avoiding” the trauma, while the “EP” is completely fixated upon the trauma (Grant, 2015). To the degree that helplessness was experienced during the traumatic incident, the individual will likely experience increased somatoform dissociation (physical dissociation like: freezing, forgetting, shutting down [catatonia], etc.) (Grant, 2015).
Somatoform dissociation is most common in survivors of childhood or early relational trauma (where the atmosphere was either physically or emotionally violent) (Grant, 2015).
There are two types of somatoform dissociation (Grant, 2015):
Type 1: Here, the focus becomes on the “felt-pain” of the physical body. By doing this, the individual avoids the emotional pain underlying the physical symptom(s). The individual often experiences unrelenting physical pain due to the misinterpretation of emotional pain as physical pain.
Type 2: Here, the individual often experiences a “stepping-out-of-the-body” (or a floating away from the body). Individuals often can notice their idealized body from a fantasy perspective (such as from the ceiling, or from across the room). This allows the individual the opportunity to divorce themselves from the physical and emotion pain experienced at the time of traumatic incident (and any time it is triggered in day-to-day living).
If Type 2 Dissociation sounds like what you experience, you might notice this as having vague complaints, and perhaps extreme anxiety related to stressors. Individuals suffering from Type 2 Dissociation may also experience health fears following unexplained symptoms (Grant, 2015). People experiencing this type of dissociation, often minimize childhood adversity if it is brought up, and may engage in self-harming behaviours (i.e. cutting, suicidal tendencies, eating disorders, addiction, etc.), overwork (could include over-exercising), and inattention to physical health (Grant, 2015).
6. Amnesia

Individuals who have experienced disruptive childhoods (abuse, neglect, etc.) often have difficulties remembering their childhoods. Because the mind fails to associate amnesia with traumatic childhood events, the individual tends to misinterpret their childhood upbringing—a result that protects the mind from painful memories, but prevents the mind from integrating those memories and properly processing them. The individual then often experiences “body memories” in the form of anxiety, pain, and distress—symptoms which prevail until the original causes are properly reprocessed and “dealt with” (Grant, 2015).
7. Re-Experiencing Symptoms

Having memories of an upsetting event in the past is normal, but individuals who have experienced traumatic events often report themselves “re-experiencing” the trauma “in real-time.” This is a “flashback” that is more than the visual representation of the event—this is the individual actually “re-experiencing” the event.
Some examples could be: the sexual abuse survivor who re-experiences pain in their pelvic region, or gastro-intestinal system; the surgical patient awakening during the operating procedure and re-experiencing the pain of surgery while lying in bed at night; the war veteran re-experiencing “gunfire” when a car backfires or a car door is slammed too hard; or the abused partner from a domestic violence altercation, feeling as if they’re “suffocating” every time they hear someone’s tone of their voice raise; etc.
If you notice that you ever “re-experience” something distressing from your past no matter how big or small, you can get relief by working with a trauma therapist. Remember: having “flashbacks” or “re-experiencing” past distressing events is part of how our neurological networks work in the brain—there’s nothing wrong with you, what you had to experience was wrong—don’t be afraid to get help.
8. The Freeze Response

The Freeze Response is when the body instinctively immobilizes itself in the face of an overwhelmingly immediate threat. Researchers believe this is incredibly adaptive due to the natural ability to heighten perception in the face of danger (i.e. by “freezing” we stop making sounds and prepare to fight or flee) (Grant, 2015).
After “surviving” the original threat through the “freeze response,” our brain essentially says, “Hey, good job! Do it the same next time!” The response then gets wired to stressors that mimic that original threat in some way (can be very obscure actually). This sort of response can be incredibly adaptive and useful for situations which are extremely similar, but unfortunately is not adaptive in day-to-day life.
Imagine for example that you were in a convenience store that gets “held-up.” The assailant is screaming at the clerk and waving a gun around. Now, your immediate response is to “freeze.” You feel the sick feeling of helplessness and fear racing through your body. In a few minutes, it’s all over and the assailant leaves. No overt harm is done to anyone. Later on, you may notice that you start to feel sick when people raise their voices, and you cannot move. Once they lower their voices, and the situation becomes “calm” again, you suddenly can move like normal, and that sick feeling is gone. That is an example of “the freeze response” in both an adaptive and maladaptive form.
If you suspect that you enter the “freeze response” while encountering a stressor (internal or external), you can be helped by working through the original trauma, with a trauma-trained specialist.
9. Internal Health Concerns

Studies have shown that individuals who have suffered “severe childhood maltreatment,” are at a 1.6 to 2.9 times greater risk for developing: ischemic heart disease, cancer, chronic lung disease, skeletal fractures, hepatitis, stroke, diabetes, and liver disease (van der Kolk, 2000). If you have been diagnosed with any of these, it might be wise for you to explore if there are any underlying trauma that can be worked through.
10. Behavioural Health Concerns

Everybody spends some time on the couch from time to time, and may even partake in the occasional recreational activities with friends or family, but those doing do excessively, may have some underlying trauma to work through.
According to (van der Kolk, 2000), people who have suffered severe childhood maltreatment are 1.4 to 1.6 times more likely to be physically inactive and to be obese, 4 to 12 times more likely to develop alcoholism, abuse drugs, and to attempt suicide; and are 2 to 4 times more likely to smoke, have 50+ sexual partners, and to contract an STI.
If you find yourself having more than the occasional drink with friends, using more than the occasional recreational drug, having many sexual partners, feeling a constant low mood, are inactive for extended periods of time, and/or begin thinking of suicide on a regular basis, please see someone ASAP. It could save your life—it did for me. Remember, these behaviours are normal responses to abnormal events that you may have encountered recently, or long ago (traumatic material does not have an expiry date).
Getting help from a trauma therapist in conjunction with your physiotherapist, massage practitioner, and/or doctor, doesn’t mean that you’re weak, or defective, or broken in any way—it means that you have the courage and self-respect to live your life how you are meant to: emotionally free and physically healthy.
If you’ve enjoyed this article, and found it helpful for you, I’d love to hear from you in the comments section. I encourage you to “like” and “share” this information if you think it can benefit anyone you know.
Visit our website to learn more about EMDR. We offer Free Consultations to see how receiving EMDR treatment could benefit you.
Works Cited
Grant, M. (2015). Pain control with EMDR: Treatment manual (5th ed.). Australia: Mark Grant
Levine, P. (1997). Waking the tiger: Healing trauma. California: North Atlantic Books.
van der Kolk, B. (2000). Posttraumatic stress disorder and the nature of trauma. Dialogues in Clinical Neuroscience, 2 (1), 7-22.
__________________________
In good health, care, and the utmost respect,